Robotic surgery systems are changing how hospitals handle complex operations.
Instead of relying solely on human hands, surgeons use robotic arms guided from a console to perform procedures with greater precision and control.
Platforms like da Vinci and Hugo have already helped make over 1.8 million surgeries possible worldwide, offering smaller incisions, faster recovery, and improved patient outcomes.
What is robotic surgery, and how does it work?
Robotic surgery, also known as robot-assisted surgery, is a minimally invasive surgical technique where a surgeon uses a robotic system to perform operations. It improves precision, flexibility, and control during complex procedures, often through smaller incisions, leading to potential benefits like less pain and faster recovery.
Example:
- Surgeon at the console: The surgeon sits at a console a few feet from the patient.
- Robotic arms: Controlled by the surgeon, fitted with miniaturized surgical instruments.
- 3D HD camera: Provides a magnified, high‑definition, three‑dimensional view of the surgical site.
- Motion translation: The surgeon’s hand movements are scaled and translated into precise robotic movements.
Robotic systems differ from AI-driven or fully autonomous robots because they require human control, especially in critical surgery.
Modern platforms like da Vinci, Versius, and Hugo come equipped with advanced software that filters out tremors, adjusts motion scaling, and even offers training modules. The entire ecosystem, from the robot arms to the interface, is integrated using specialized protocols.
In some hospitals, these systems are also being used for remote surgeries or telesurgery, where the surgeon might control the robot from another room or even another city with latency-free feedback.
Common robotic surgery procedures
While it first gained traction in urology and gynecology, its use has expanded to general surgery, cardiac procedures, thoracic operations, ENT (ear, nose, throat), and even oncology.
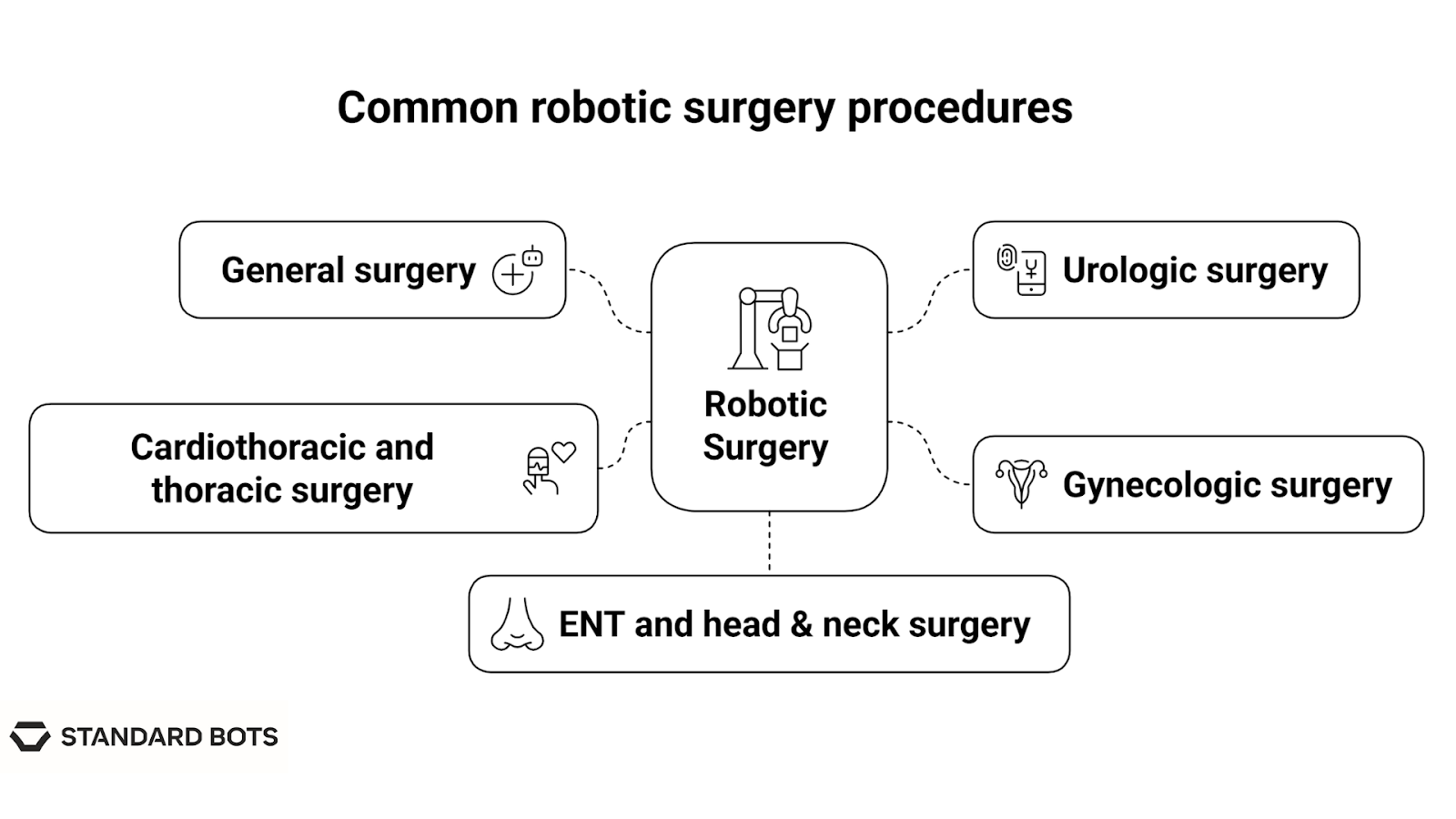
Here are the primary domains where robotic systems are most commonly used:
1. General surgery
Robotic platforms are increasingly used for everyday healthcare procedures that were traditionally open or laparoscopic.
- Gallbladder removal (cholecystectomy), where the robot allows better visualization of the bile duct and surrounding structures.
- Hernia repair, including inguinal, ventral, and hiatal, where enhanced articulation helps with mesh placement and suturing.
- Bariatric surgery, like sleeve gastrectomy or gastric bypass, where a robot that helps maintain precision across multiple staple lines and reduces tissue trauma.
2. Urologic surgery
Urology was one of the earliest adopters of robotic assistance. It’s still the specialty with the highest number of robotic procedures performed worldwide.
- Radical prostatectomy, where the surgeon removes the prostate while preserving nerves critical for continence and sexual function.
- Partial nephrectomy, where only the tumor portion of a kidney is removed, sparing the rest of the organ.
- Bladder surgery, including tumor resection and reconstruction.
The confined space of the pelvis makes robotic precision especially valuable in these procedures, allowing surgeons to work around critical nerves and vessels with minimal damage.
3. Gynecologic surgery
Gynecologists use robotic systems for delicate dissections and extensive suturing, especially in patients with prior surgeries or endometriosis.
- Hysterectomy, where robotic assistance enables a clearer view of the uterus, ovaries, and nearby structures.
- Myomectomy, which involves the removal of fibroids from the uterus, is often performed with reconstruction.
- Endometriosis excision for deep pelvic lesions.
4. Cardiothoracic and thoracic surgery
Operating in the chest cavity is challenging due to limited space and critical organs. Robotic platforms have made minimally invasive heart and lung surgeries more accessible.
- Coronary artery bypass (in selected patients) avoids full sternotomy.
- Lung biopsies and lobectomies, especially indicated in early-stage cancer.
- Mitral valve repair, where the robot helps with delicate tissue handling and intracardiac suturing.
5. ENT and head & neck surgery
Robotic systems are also used in select procedures involving the throat, mouth, and thyroid:
- Transoral robotic surgery (TORS) allows surgeons to access tumors at the base of the tongue or tonsils without splitting the jaw or making external incisions.
- Thyroidectomy, where robotic tools allow the removal of the thyroid gland through an incision in the armpit or behind the ear to avoid neck scars.
For a side-by-side breakdown, see laparoscopic vs robotic surgery, where we compare the tools, outcomes, and use cases of each method.
Benefits of robotic surgery for patients and surgeons
Robotic surgery is gaining popularity because the outcomes speak for themselves. Using these tools makes surgery less traumatic, more precise, and easier to recover from.
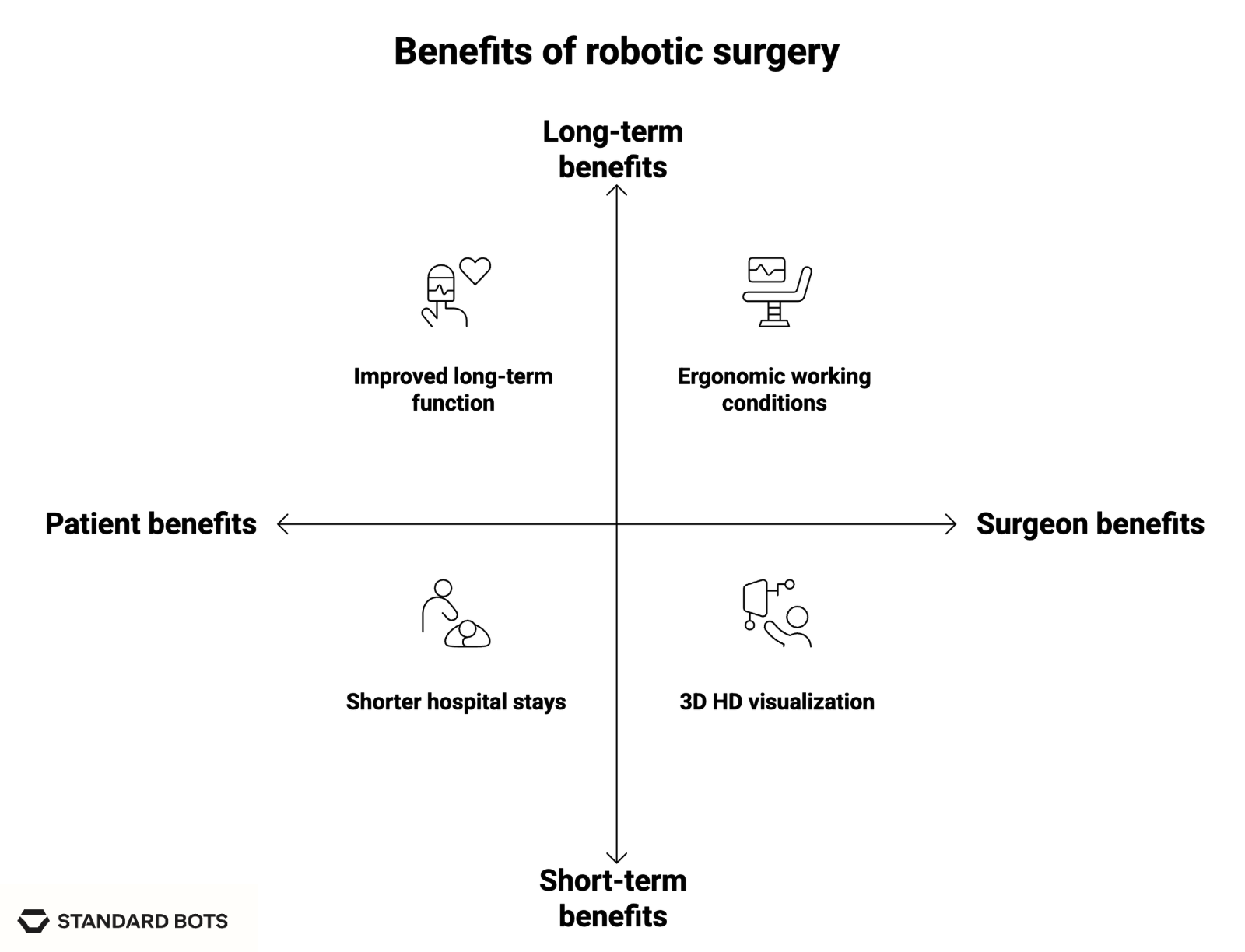
For patients
- Smaller incisions: Robotic instruments typically require incisions smaller than 1 cm. Less cutting means less disruption to skin, muscle, and fascia, which translates to fewer complications.
- Lower risk of infection and blood loss: Because the entry points are smaller and the precision is higher, there’s less internal bleeding and a lower chance of surgical site infections.
- Shorter hospital stays: A large portion of patients who undergo robotic surgery are discharged within 24 to 48 hours.
- Less postoperative pain: Fewer and smaller incisions result in reduced use of narcotic pain medications, helping patients avoid common side effects.
- Improved long-term function: In urologic and gynecologic surgeries, especially, preserving nerve and organ function is critical. The precision of robotic systems helps minimize long-term side effects like incontinence or sexual dysfunction.
For surgeons
- Ergonomic working conditions: Surgeons operate from a seated console with hand, wrist, and foot controls. This reduces physical strain, especially in long procedures.
- 3D HD visualization: Unlike traditional laparoscopy’s 2D view, robotic systems offer a high-definition, three-dimensional image that can be zoomed and adjusted for a clear look at tissues and vessels.
- Tremor filtration and motion scaling: The system converts large hand movements into micro-instrument adjustments, perfect for delicate suturing or dissection near vital nerves.
- Greater dexterity inside the body: Robotic wrists mimic the motion range of a human hand but can also rotate 540 degrees in some models. This makes it possible to reach and operate in tight or curved spaces that straight laparoscopic tools can’t access.
Limitations and considerations of robotic surgery
1. High costs of acquisition and maintenance
A flagship platform like da Vinci Xi can cost between $1.5 to $2 million, not including:
- Disposable instruments that need replacing every few uses
- Annual maintenance contracts, which often run into six figures
- Training and credentialing programs for surgeons and support staff
These expenses can put robotic surgery out of reach for smaller hospitals, especially in rural or underfunded regions.
2. Longer setup and operating room (OR) times
Although robotic procedures tend to be efficient once surgeons are experienced, the setup and docking time for the robot can slow down the process. Positioning the robotic arms, calibrating instruments, and ensuring sterile conditions takes longer than simply starting a laparoscopic case.
3. Steep learning curve for surgeons
Robotic systems require dedicated training. Even experienced laparoscopic surgeons need time to adjust to:
- Using wristed instruments effectively
- The console interface and foot pedal controls
- Navigating without tactile feedback (most current systems lack haptics)
Studies show that it can take 20 to 40 cases before a surgeon becomes proficient in certain robotic procedures.
4. Not suitable for all patients or surgeries
Some surgical scenarios aren’t ideal for robotic intervention:
- Very large tumors may require open surgery due to size or location
- Emergency cases, where time is critical, may not allow for a robotic setup
- Extensive internal scarring from prior surgeries can make robotic access difficult
- Patients with certain health conditions (e.g., severe cardiopulmonary disease) might not tolerate the longer procedure time or positioning requirements
5. Uncertain insurance coverage and reimbursement gaps
In many health systems, robotic procedures are reimbursed at the same rate as laparoscopic surgery, despite the higher equipment and supply costs. This gap puts financial pressure on hospitals and may limit how often the robot is used.
In countries with private insurance, coverage varies widely. Some plans consider robotic surgery medically necessary; others classify it as optional or experimental, leaving patients to cover part or all of the cost.
How robotic surgery fits into modern healthcare
Robotic surgery is becoming a foundational tool in how modern hospitals operate. These systems offer a scalable, precise, and increasingly essential solution to today’s healthcare challenges.
1. Meeting surgical demand in high-volume centers
In busy urban hospitals, surgeons perform dozens of complex procedures weekly.
Robotic systems help:
- Standardize outcomes, reducing variation between surgeons
- Lower complication rates, which frees up beds and reduces readmission
- Improve workflow efficiency through better ergonomics and task automation
For example, when robotic surgery is used in colorectal procedures, studies show fewer conversions to open surgery, which leads to shorter hospital stays and better postoperative recovery.
2. Extending surgical access to rural and remote regions
One of the most exciting applications of robotic surgery is telesurgery. With the right infrastructure, a skilled surgeon can operate remotely, guiding robotic instruments located miles or even continents away.
While still in early phases, remote robotic surgery has already been trialed successfully. As network speeds and real-time feedback systems improve, it’s becoming more viable for rural hospitals to offer advanced procedures without needing full-time specialists on site.
3. Supporting surgical education and resident training
Robotic systems come with built-in simulation tools and learning environments, helping new surgeons build skills without risking patient safety.
This is especially valuable in teaching hospitals, where:
- Recorded procedures can be used for review and feedback
- Dual consoles allow instructors to take control mid-procedure
- Metrics like motion tracking and instrument use help assess performance
Residents trained on robotic platforms often gain confidence earlier in their careers, leading to faster skill development and broader surgical competency.
4. Supporting system-wide digital transformation
Hospitals are shifting toward more integrated digital ecosystems, and surgical robotics fits directly into that trend.
These systems are being designed to:
- Sync with electronic health records (EHRs)
- Integrate with operating room scheduling platforms
- Work alongside AI-driven analytics to track outcomes and improve protocols
The result is a more connected operating room that captures data, improves decisions, and supports continuous improvement across departments.
As healthcare systems deal with staffing shortages and rising caseloads, robotic platforms can help deliver better care with fewer complications. For example, compact units like the UR3 robot are being explored for modular use, training labs, and outpatient settings.
The future of robotic surgery
Several technologies are making these systems smarter, more affordable, and more capable. The goal here is better outcomes, better training, and broader accessibility.
1. AI-assisted decision-making in real time
Surgeons already use preoperative imaging and planning software, but the next step is real-time support.
Artificial intelligence is being trained to:
- Recommend instrument paths based on preloaded 3D models
- Alert the surgeon if pressure, angle, or temperature readings deviate from safe norms
- Flag anatomical structures during procedures (e.g., nerves, blood vessels, tumor margins)
While AI won’t replace surgical decision-making, it’s starting to act like a co-pilot, enhancing awareness and catching errors before they happen.
2. Pre-op simulations and digital twin modeling
Before a scalpel ever touches a patient, robotic systems will increasingly use patient-specific simulations. Surgeons will be able to rehearse entire procedures in virtual environments, adjusting for unique anatomy or surgical challenges.
These “digital twins” will integrate CT/MRI data with AI-generated tissue models, allowing for more tailored surgical planning.
3. Advanced haptics and tactile feedback
One of the current limitations of robotic surgery is the lack of haptic feedback: the sense of touch. Most systems rely entirely on visual cues.
Newer platforms are beginning to restore this by:
- Using force sensors in robotic arms
- Displaying real-time pressure data on instruments
- Translating resistance into vibrations or pressure at the surgeon’s console
This tactile input is particularly important in procedures that involve delicate dissection or require nuanced pressure, like vascular repairs or pediatric surgeries.
4. Voice-activated controls
Surgeons are already navigating complex instrument controls with hand and foot pedals.
Shortly, voice-assisted interfaces could allow:
- Quick instrument changes
- Adjustments in camera position
- Activation of specific robotic arms or functions
5. Integration of novel robotic functions, like robotic extrusion
One of the most exciting new frontiers is the integration of robotic extrusion that enables robots to deposit biological or synthetic material layer by layer.
This has potential applications in:
- Burn treatment, where robots apply skin substitutes precisely over damaged areas
- Reconstructive surgery, where tissue scaffolds or implants are built directly inside the body
- Orthopedics, where bone cement or structural materials are robotically placed with micrometer-level control
Final Take
Robotic surgery combines the skill of a trained surgeon with the precision of robotic tools, offering better results, faster recovery, and less strain. While it isn’t a fit for every procedure or patient, its advantages are undeniable in specific specialties like urology, gynecology, and cardiac surgery.
As the technology matures and becomes more affordable, robotic systems will become as standard as scalpels once were.
Which robot offers surgical-level accuracy for industrial automation?
Standard Bots brings that same commitment to precision and reliability to industrial applications. RO1 offers surgical-level accuracy, helping manufacturers achieve consistent results in their operations.
- Affordable and adaptable: RO1 costs $37K list price. Get high-precision automation at half the cost of traditional robots.
- Precision and power: With a repeatability of ±0.025 mm and an 18 kg payload, RO1 handles even the most demanding CNC jobs.
- AI-driven simplicity: Equipped with AI capabilities on par with GPT-4, RO1 integrates seamlessly with CNC systems for advanced automation.
- Safety-first design: Machine vision and collision detection mean RO1 works safely alongside human operators.
Schedule your on-site demo with our engineers today and see how RO1 can bring AI-powered greatness to your shop floor.
FAQs
1. What is robotic surgery, and how is it performed?
Robotic surgery is a form of minimally invasive surgery where a human surgeon operates robotic arms using a console. The system translates the surgeon’s hand movements into highly precise instrument motions. A 3D camera inserted into the patient provides a magnified view of the surgical site, allowing for better accuracy than standard laparoscopic tools.
2. What procedures are commonly done using robotic systems?
Procedures commonly done using robotic systems include general surgery, urology, gynecology, thoracic surgery, and oncology. Some of the most common procedures include prostate removal, hysterectomy, gallbladder surgery, hernia repair, kidney surgery, and mitral valve repair.
3. What are the main benefits for patients and doctors?
The main benefits for patients of robotic surgery are smaller incisions, reduced blood loss, fewer complications, and faster recovery. For surgeons, benefits include better visibility through high-definition 3D imaging, enhanced instrument control with tremor reduction, and improved ergonomics during long procedures.
4. Are there any risks or downsides to robotic surgery?
Downsides to robotic surgery are that it is expensive to purchase and maintain, and it requires significant training. Not all procedures are ideal for robotic assistance, especially emergencies or cases with extensive internal scarring.
5. How is robotic surgery different from laparoscopic surgery?
Robotic surgery is different from laparoscopic surgery because laparoscopic tools are rigid and controlled directly by the surgeon’s hands, whereas robotic instruments are wristed and can mimic the full range of human motion.
6. Is robotic surgery more expensive, and is it covered by insurance?
Robotic surgery is more expensive due to the equipment and disposable tools used, along with higher maintenance fees. Whether insurance covers it depends on the country, insurer, and type of surgery. Patients are encouraged to check with their providers before scheduling robotic procedures.
7. What role will AI and automation play in future surgical robotics?
AI is expected to enhance robotic surgery by supporting real-time decision-making, improving surgical planning, and automating routine tasks like suturing or retraction. However, fully autonomous robotic surgery remains experimental, and human surgeons will remain central to most procedures for the foreseeable future.
Join thousands of creators
receiving our weekly articles.